Rxbenefits Prior Authorization Form
Rxbenefits Prior Authorization Form - Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. These reviews are meant to ensure. This information can be obtained by contacting your prescribing physician. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Before you get started, in addition to your insurance card, you will need the following information. This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851.
A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. Before you get started, in addition to your insurance card, you will need the following information. These reviews are meant to ensure. Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851. This information can be obtained by contacting your prescribing physician.
Before you get started, in addition to your insurance card, you will need the following information. This information can be obtained by contacting your prescribing physician. This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851. These reviews are meant to ensure. Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call.
Top Digital Prior Authorization Companies AVIA Marketplace Resources
Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Before you get started, in addition to your insurance card, you will need the following information. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being.
Fillable Online MEDICATION PRIOR AUTHORIZATION REQUEST FORM
This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851. Before you get started, in addition to your insurance card, you will need the following information. Each time one of our representatives answers the phone, the goal.
Fillable Online Vidaza CCRD Prior Authorization Form. Prior
Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. This can be located on your medical id card (if you have.
Medicare Update Prior Authorization Request Process for Certain
Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Before you get started, in addition to your insurance card, you will need the following information. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first.
Prior Authorization Nurse Healthcare Support
This information can be obtained by contacting your prescribing physician. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. This can.
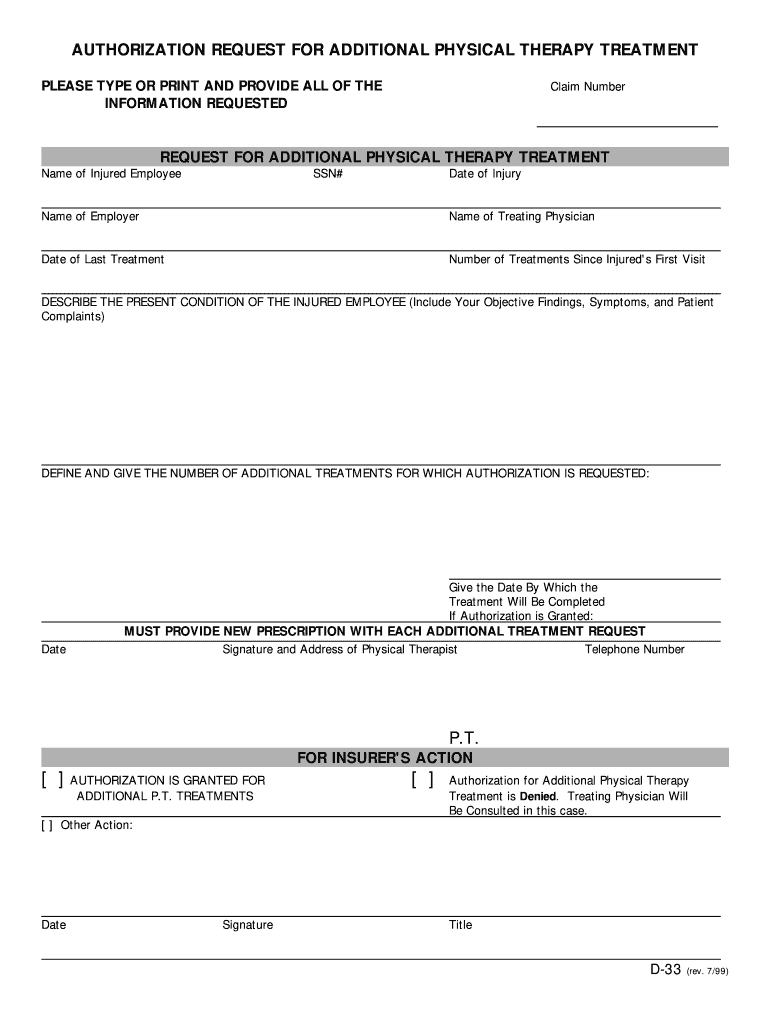
Authorization Request for Additional Physical Therapy Form Fill Out
Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851. A prior.
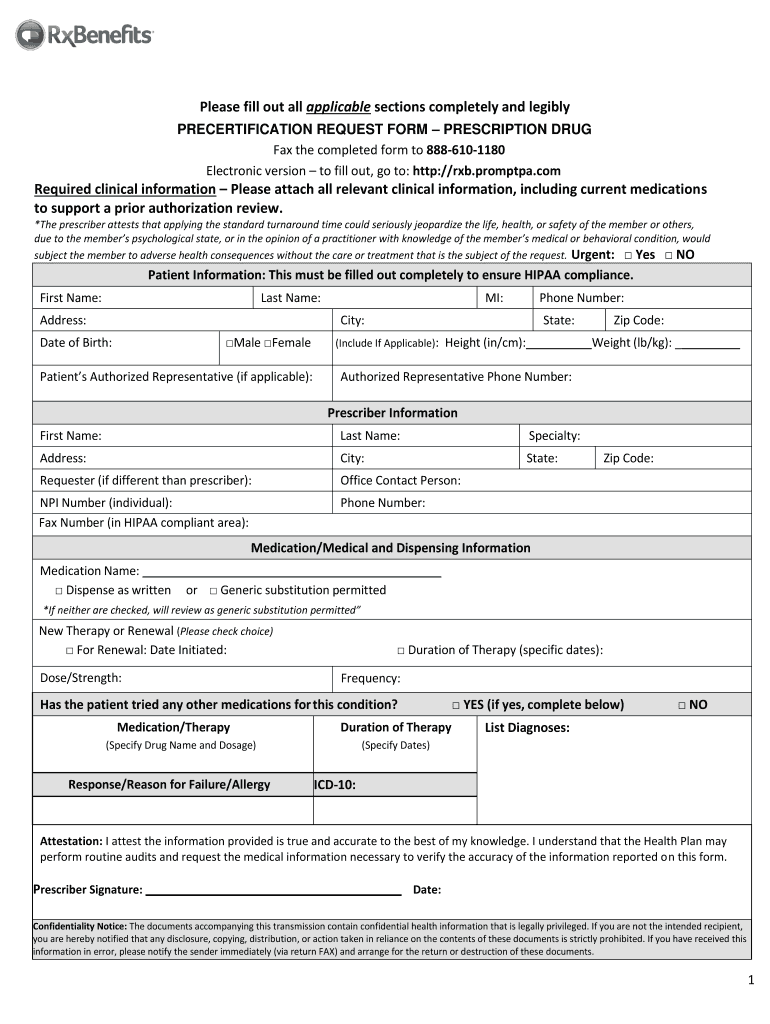
Prior Authorization Form Download RxBenefits
Before you get started, in addition to your insurance card, you will need the following information. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Your fastest form of contact to resolve your issue will be to log into your my.
Efficient Ways to Handle Prior Authorization Process
Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. This information can be obtained by contacting your prescribing physician. Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Before you get started, in.
Rxb Promptpa Com Complete with ease airSlate SignNow
This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851. A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda.
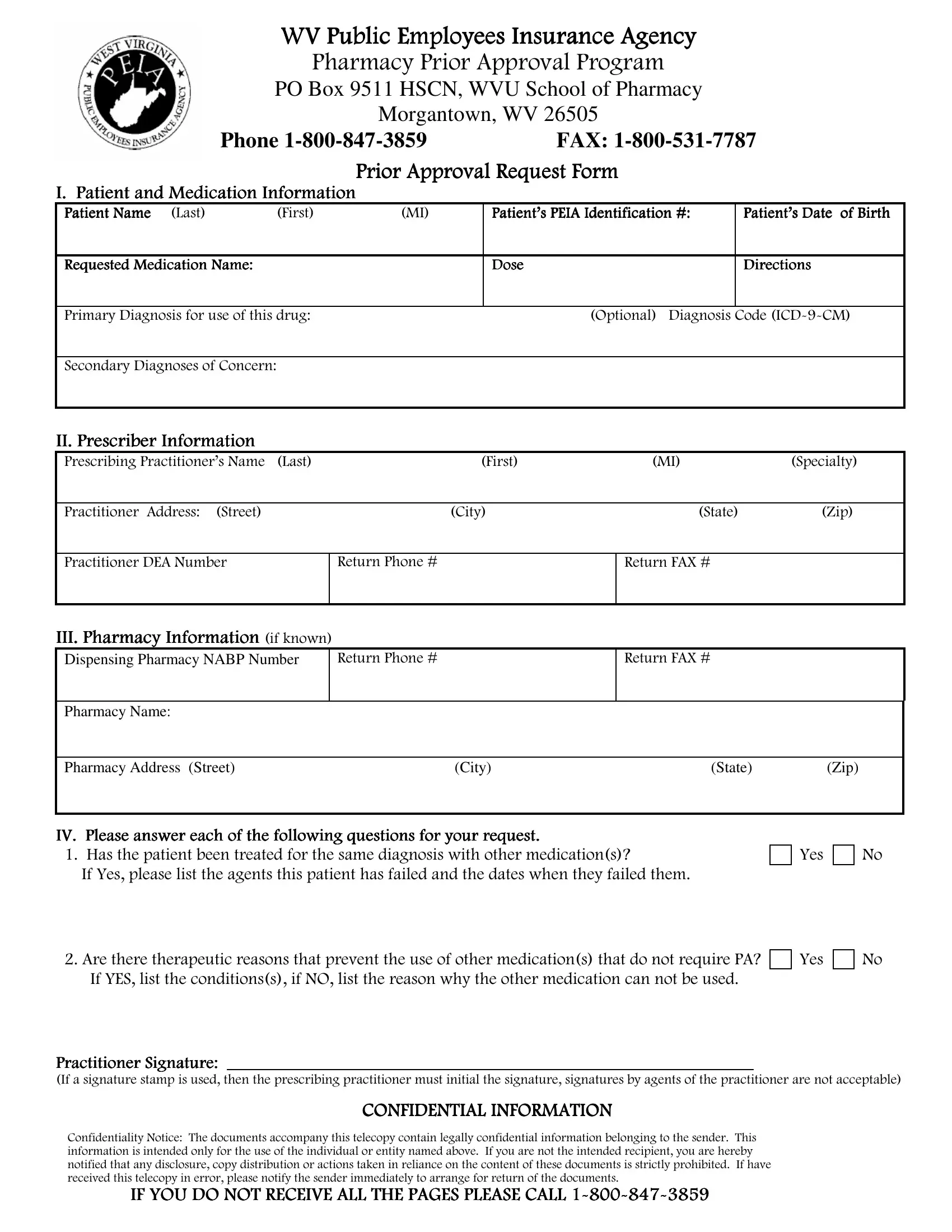
Wv Peia Prior Authorization PDF Form FormsPal
Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call. A prior authorization (pa) review is used for a wide variety of medications to confirm.
These Reviews Are Meant To Ensure.
A prior authorization (pa) review is used for a wide variety of medications to confirm that medication is being prescribed for its intended use based on fda guidelines. Before you get started, in addition to your insurance card, you will need the following information. Your fastest form of contact to resolve your issue will be to log into your my rxbenefits portal or email member services team at customercare@rxbenefits.com. Each time one of our representatives answers the phone, the goal is simple—resolve our member’s issue on the first call.
This Information Can Be Obtained By Contacting Your Prescribing Physician.
This can be located on your medical id card (if you have a combined medical and pharmacy card), on your pharmacy card, or by calling the member services prior authorization line at 888.608.8851.