Optum Rx Appeal Form
Optum Rx Appeal Form - Optum rx prior authorization department p.o. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. If denied, the provider may. Download the form below and mail or fax it to unitedhealthcare: Optum rx c/o appeals coordinator p.o. Once a review is complete, the provider is informed whether the pa request has been approved or denied.
Optum rx c/o appeals coordinator p.o. Once a review is complete, the provider is informed whether the pa request has been approved or denied. Optum rx prior authorization department p.o. Download the form below and mail or fax it to unitedhealthcare: If denied, the provider may. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal.
Optum rx prior authorization department p.o. If denied, the provider may. Optum rx c/o appeals coordinator p.o. Download the form below and mail or fax it to unitedhealthcare: Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. Once a review is complete, the provider is informed whether the pa request has been approved or denied.
Fillable Online Determination of Bid Protest SF20150160. Response to
Once a review is complete, the provider is informed whether the pa request has been approved or denied. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. Optum rx c/o appeals coordinator p.o. Download the form below and mail or fax it to unitedhealthcare: If denied, the provider may.
Optum Health Claim Form
If denied, the provider may. Optum rx prior authorization department p.o. Download the form below and mail or fax it to unitedhealthcare: Optum rx c/o appeals coordinator p.o. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal.
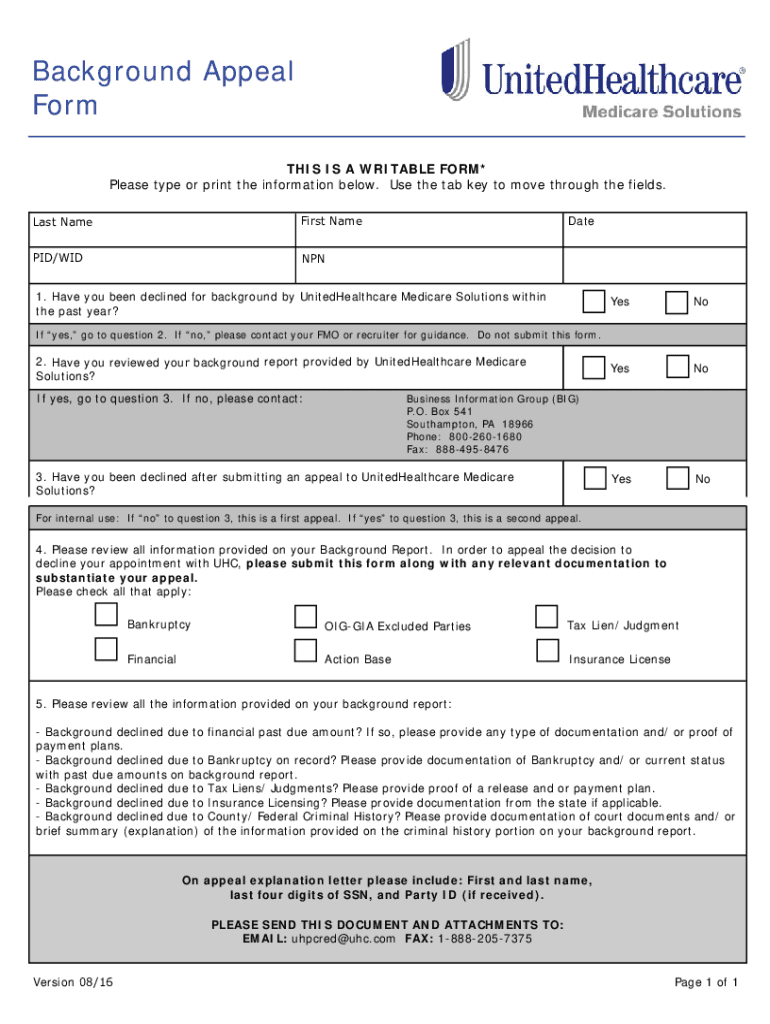
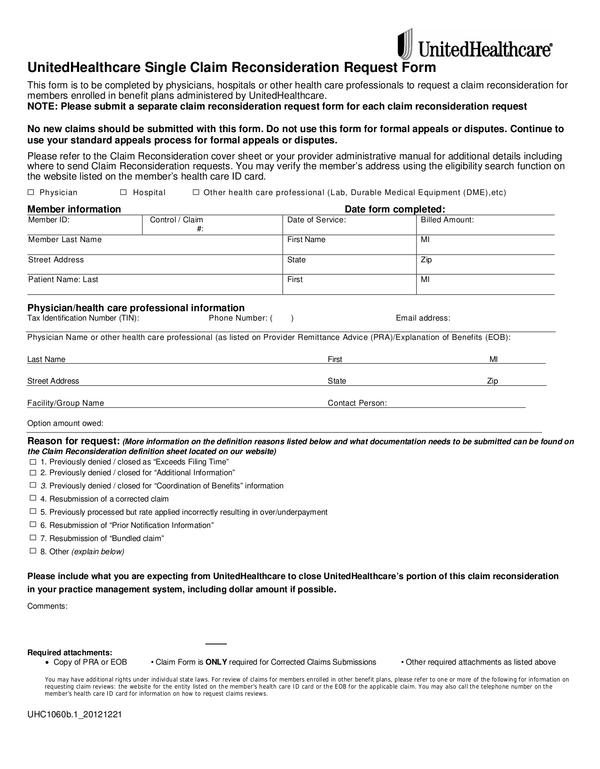
United Healthcare Provider Appeal 20162024 Form Fill Out and Sign
Optum rx c/o appeals coordinator p.o. Optum rx prior authorization department p.o. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. Once a review is complete, the provider is informed whether the pa request has been approved or denied. If denied, the provider may.
OptumRX Humble ISD
Once a review is complete, the provider is informed whether the pa request has been approved or denied. Optum rx c/o appeals coordinator p.o. Optum rx prior authorization department p.o. Download the form below and mail or fax it to unitedhealthcare: Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal.
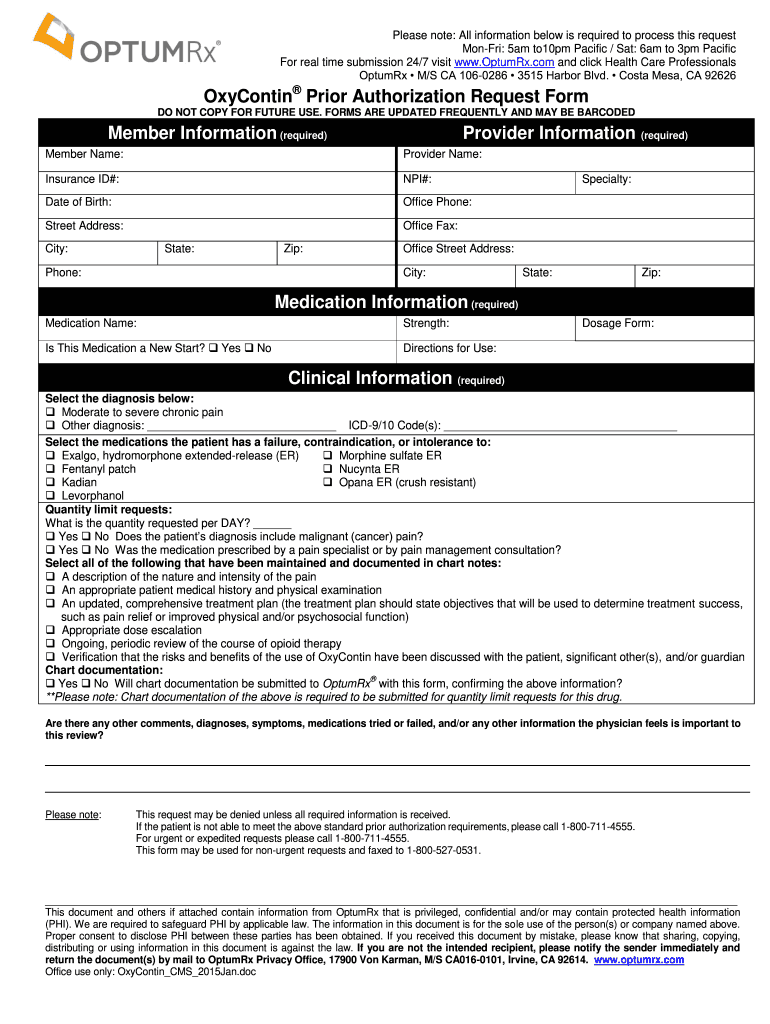
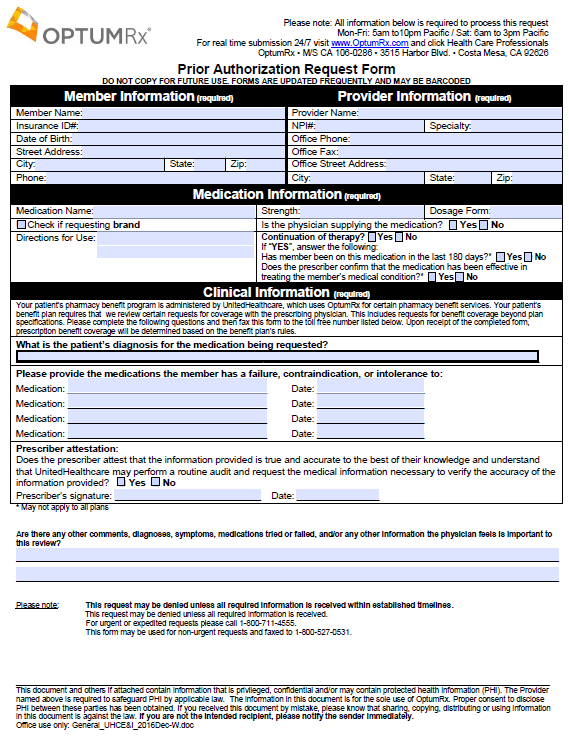
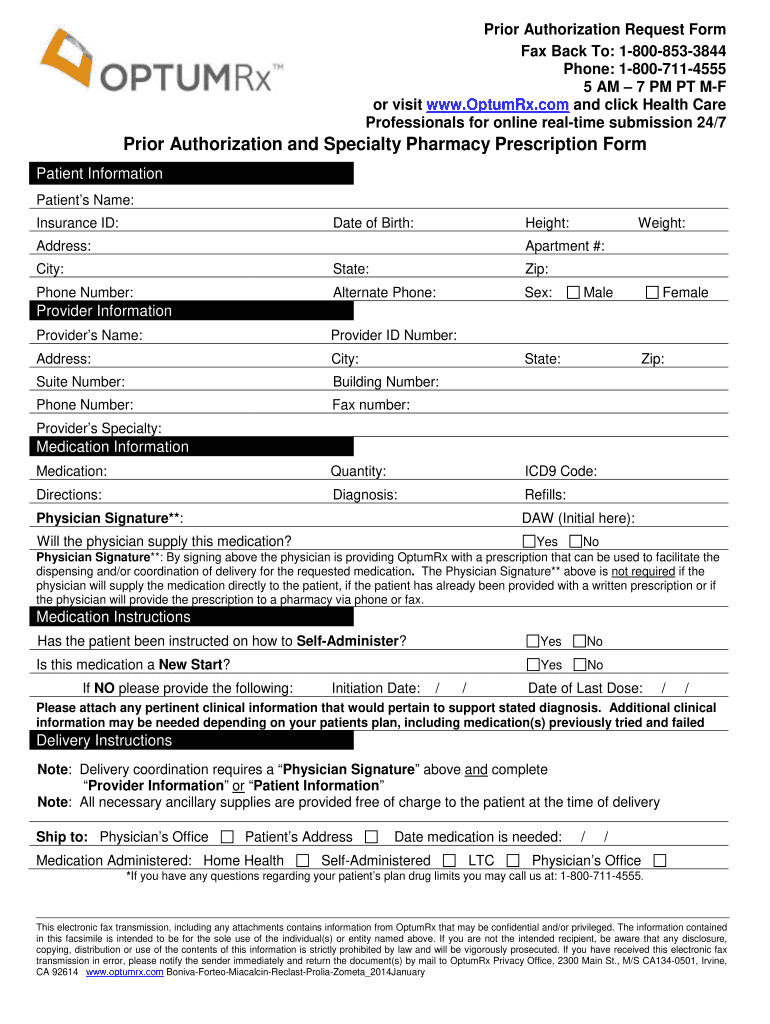
Fillable Online Prior Authorization Request Form (Page 1 of 2)Go
Download the form below and mail or fax it to unitedhealthcare: Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. If denied, the provider may. Optum rx c/o appeals coordinator p.o. Optum rx prior authorization department p.o.
Top United Healthcare Appeal Form Templates Free To Download In PDF
Optum rx c/o appeals coordinator p.o. Download the form below and mail or fax it to unitedhealthcare: Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. Optum rx prior authorization department p.o. If denied, the provider may.
Optumrx Appeal PDF 20152024 Form Fill Out and Sign Printable PDF
If denied, the provider may. Optum rx prior authorization department p.o. Optum rx c/o appeals coordinator p.o. Download the form below and mail or fax it to unitedhealthcare: Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal.
Free OptumRX Prior Prescription (Rx) Authorization Form PDF
If denied, the provider may. Optum rx prior authorization department p.o. Download the form below and mail or fax it to unitedhealthcare: Once a review is complete, the provider is informed whether the pa request has been approved or denied. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal.
Optum Rx Appeal Form Complete with ease airSlate SignNow
Optum rx c/o appeals coordinator p.o. Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. If denied, the provider may. Download the form below and mail or fax it to unitedhealthcare: Optum rx prior authorization department p.o.
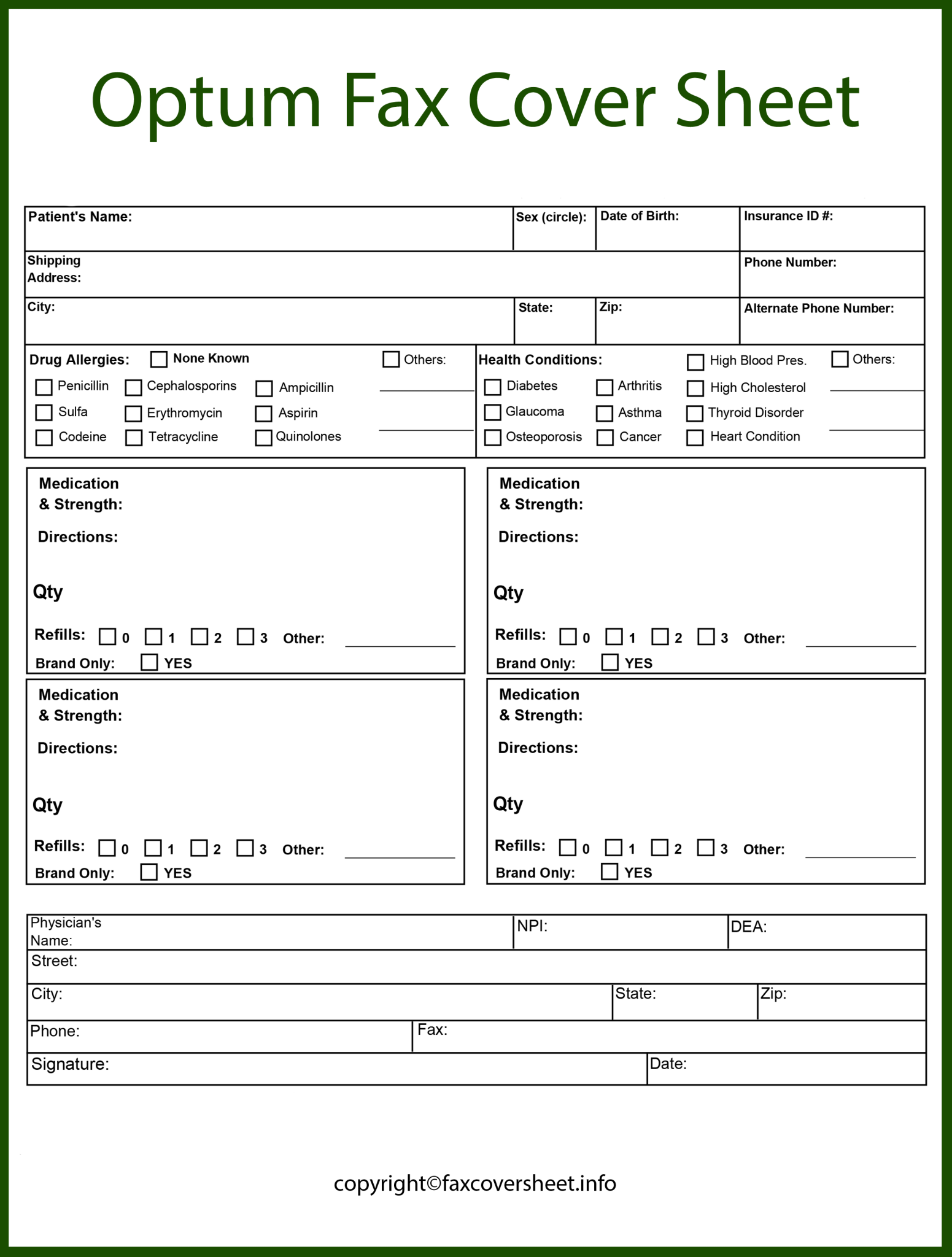
Optum Fax Cover Sheet Templates Printable in PDF & Word
Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. If denied, the provider may. Optum rx prior authorization department p.o. Once a review is complete, the provider is informed whether the pa request has been approved or denied. Download the form below and mail or fax it to unitedhealthcare:
Once A Review Is Complete, The Provider Is Informed Whether The Pa Request Has Been Approved Or Denied.
Learn how to submit mac appeals for optumrx claims using the approved spreadsheet via the pharmacy portal. Optum rx c/o appeals coordinator p.o. Download the form below and mail or fax it to unitedhealthcare: If denied, the provider may.