Humana Tier Exception Form
Humana Tier Exception Form - Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms. (1) formulary or preferred drug(s). This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Find out the types of exceptions, the. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. What is a tier exception?
(1) formulary or preferred drug(s). This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms. Find out the types of exceptions, the. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. What is a tier exception? This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: Learn how to request a coverage determination or an exception for a prescription drug covered by careplus.
This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. What is a tier exception? Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: (1) formulary or preferred drug(s). Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Find out the types of exceptions, the. Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms.
Fillable Online Humana Formulary Tier Exception. Humana Formulary Tier
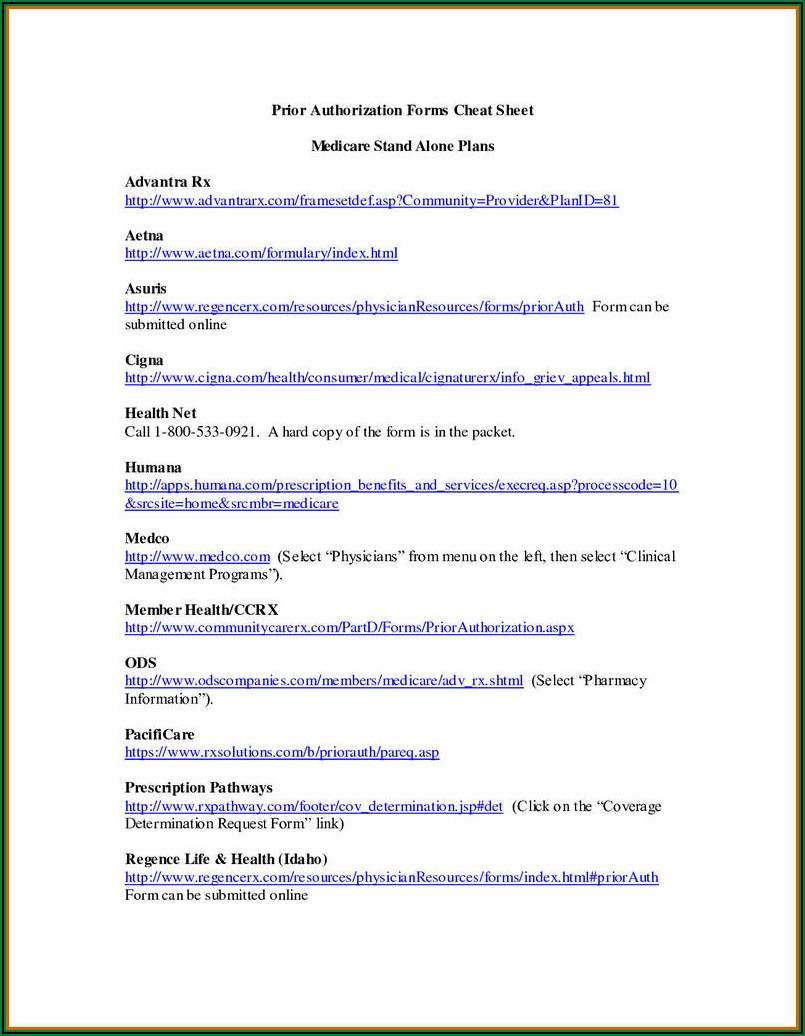
Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. What is a tier exception? Request for formulary tier exception.
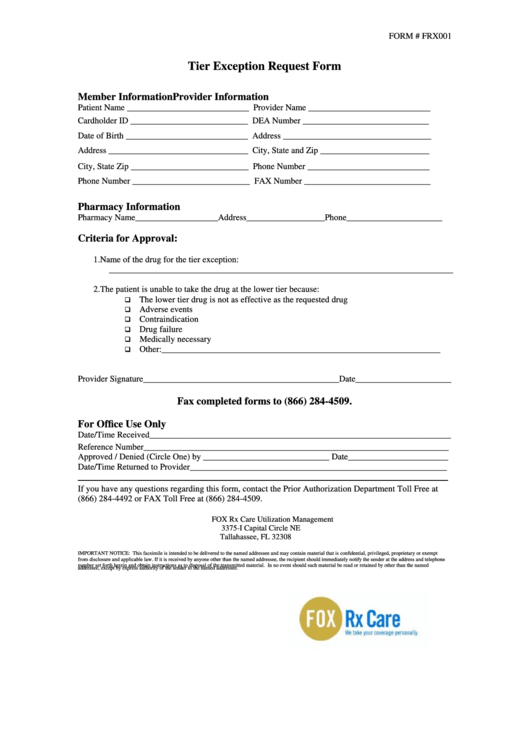
Form Frx001 Tier Exception Request Form printable pdf download
(1) formulary or preferred drug(s). This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. What is a tier exception?.
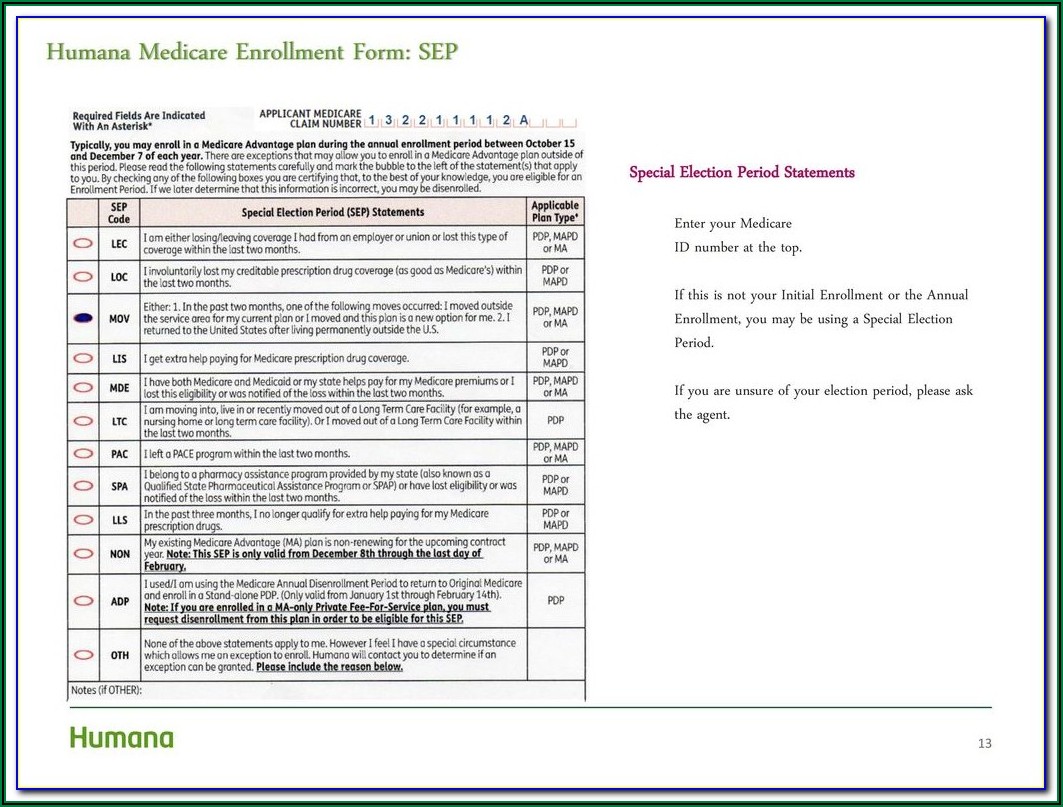
Humana Enrollment Form Pdf Form Resume Examples MW9pBy8ZVA
Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. This form is used to request a coverage determination for a prescription drug that is not.
Cvs Caremark Brand Exception Form 20202022 Fill and Sign Printable
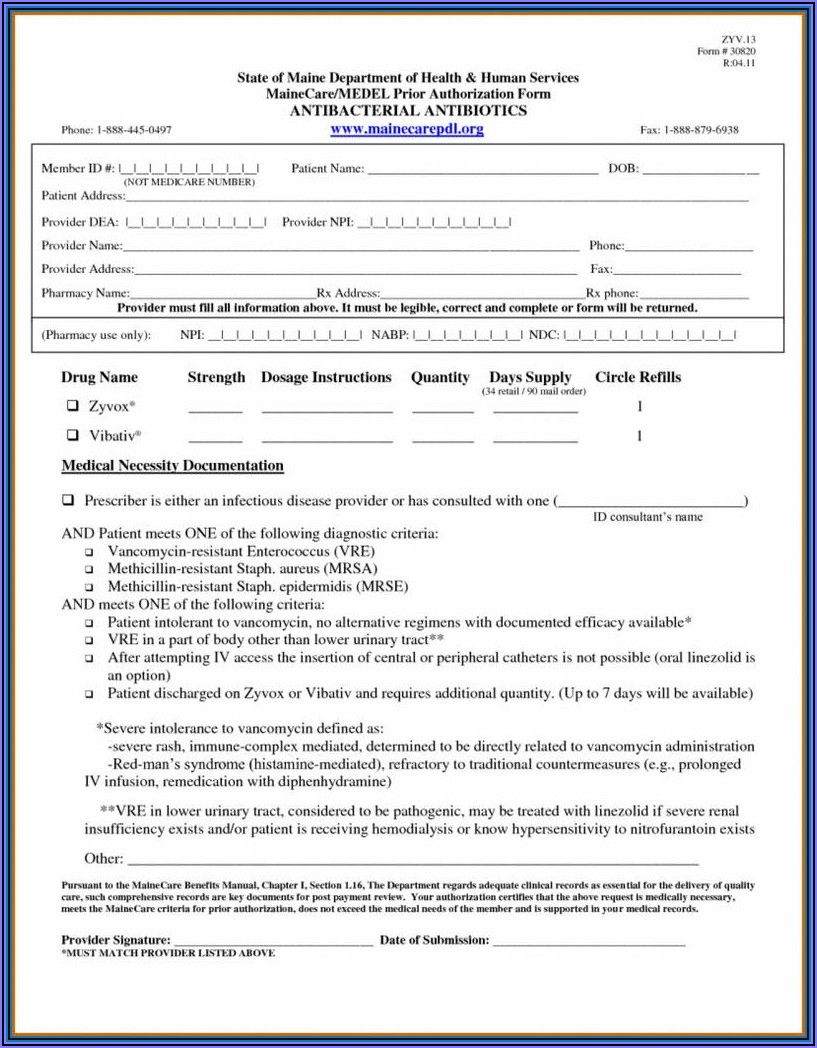
Find out the types of exceptions, the. This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. (1) formulary or preferred drug(s). This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a.
Fillable Online Request Form Tier Exception Fax Email Print pdfFiller
This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. Find out the types of exceptions, the. Providers should request a tiering exception if they want humana to.
Humana Medicare Enrollment Form Form Resume Examples 1ZV8a05023
(1) formulary or preferred drug(s). Find out the types of exceptions, the. Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Whether you're a humana.
Humana Medicare Advantage Waiver Of Liability Form Form Resume
Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. What is a tier exception? Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. This form is used to request a coverage determination for a prescription drug.
Wellcare Tier Exception Form 2024 Rafa Othelia
Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms. Providers should request.
Medicare Part D Tier Exception Form Form Resume Examples
Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms. Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs. This form is used to request a coverage determination for a prescription drug that.
Fillable Online Humana tier exception request form pdf. Humana tier
This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment. Whether you're a humana medicare member or you get insurance from your employer, you have easy access to documents and forms. Find out the types of exceptions, the. Request for formulary tier exception specify below.
Whether You're A Humana Medicare Member Or You Get Insurance From Your Employer, You Have Easy Access To Documents And Forms.
Find out the types of exceptions, the. (1) formulary or preferred drug(s). What is a tier exception? Providers should request a tiering exception if they want humana to cover a nonpreferred drug at the same cost share that would apply to drugs.
This Form Is Used To Request A Coverage Determination For A Prescription Drug That Is Not On The Plan's Formulary Or Has A Higher Copayment.
Learn how to request a coverage determination or an exception for a prescription drug covered by careplus. Request for formulary tier exception specify below if not noted in the drug history section earlier on the form: This form is used to request a coverage determination for a prescription drug that is not on the plan's formulary or has a higher copayment.