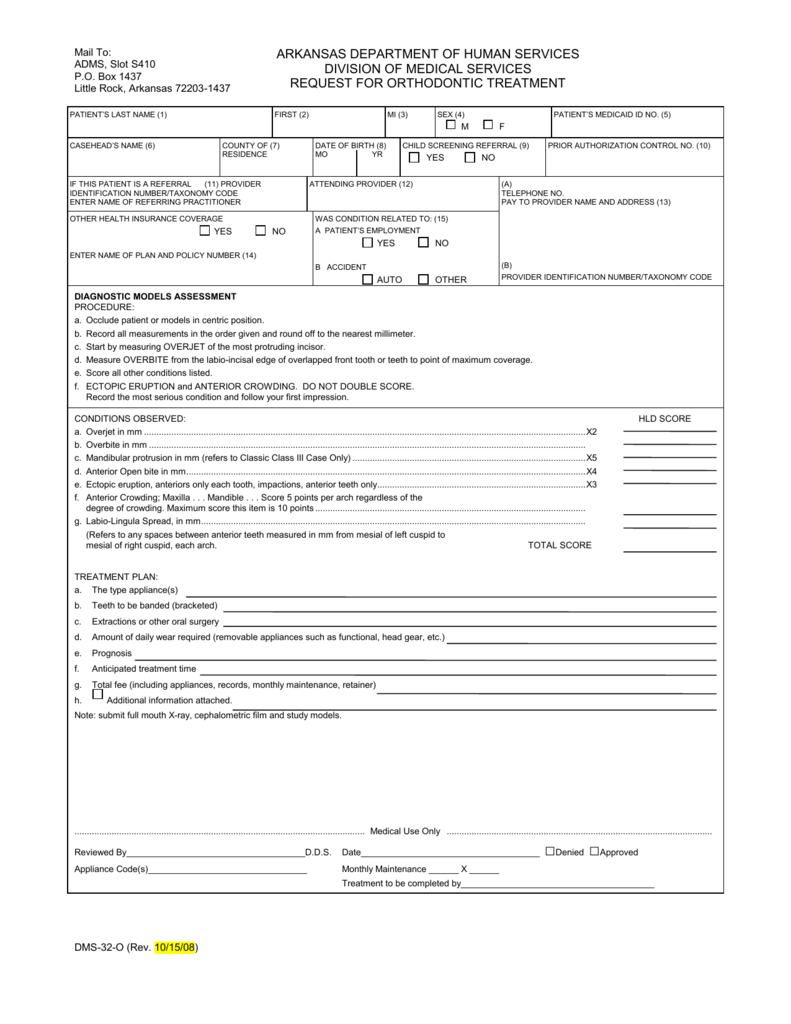
Arkansas Medicaid Prior Authorization Form
Arkansas Medicaid Prior Authorization Form - Select type of account and. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Others are added as they become. Some of the forms used by arkansas medicaid and its providers are available in electronic format. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Member must be eligible at the time services are rendered. Services must be a covered health plan benefit and medically necessary with prior.
Some of the forms used by arkansas medicaid and its providers are available in electronic format. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Select type of account and. Others are added as they become. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered.
Some of the forms used by arkansas medicaid and its providers are available in electronic format. Select type of account and. Services must be a covered health plan benefit and medically necessary with prior. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Member must be eligible at the time services are rendered. Others are added as they become. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal.
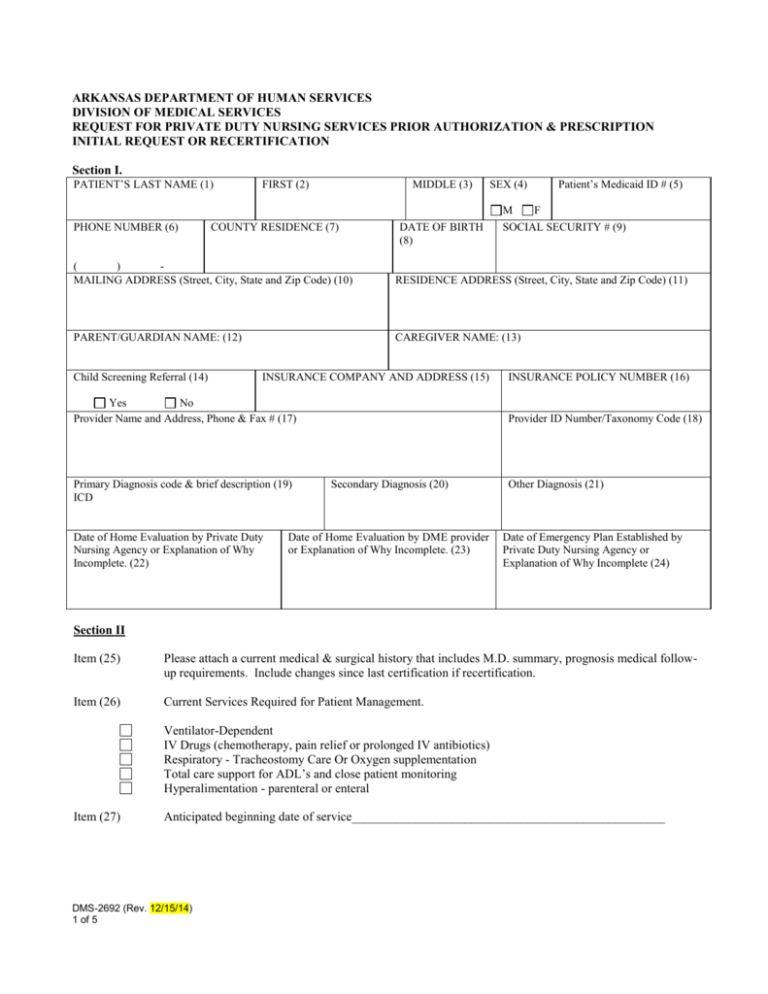
DMS320 Arkansas Medicaid
Member must be eligible at the time services are rendered. Others are added as they become. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Services must be a covered health plan benefit and medically necessary with prior. Select type of account and.
Medicaid Consent Form For Sterilization 2024 Printable Consent Form 2022
Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Services must be a covered health plan benefit and medically necessary with prior. Some of the forms used by arkansas medicaid and its providers are available in electronic format. Others are added as they become. Select type of account and.
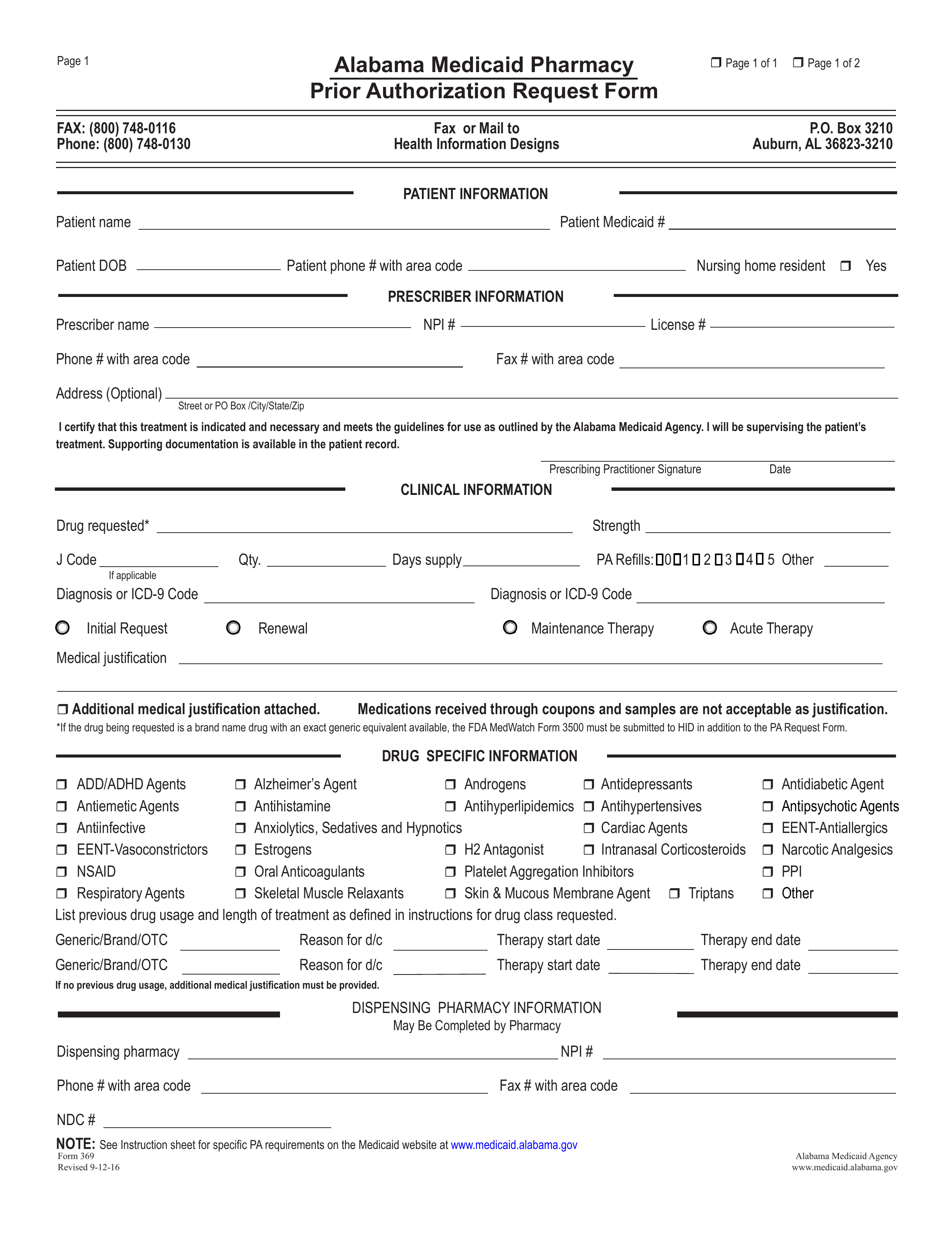
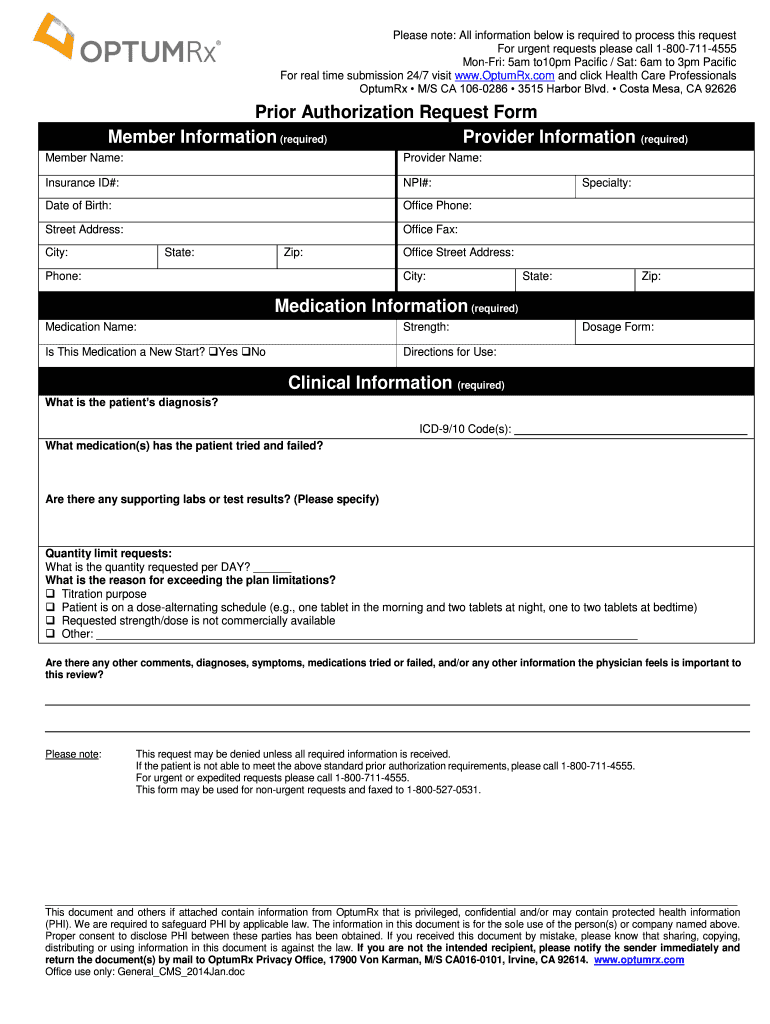
Free Alabama Medicaid Prior (Rx) Authorization Form PDF eForms
Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Select type of account and. Services must be a covered health plan benefit and medically necessary with prior. Others are added as they become. Member must be eligible at the time services are rendered.
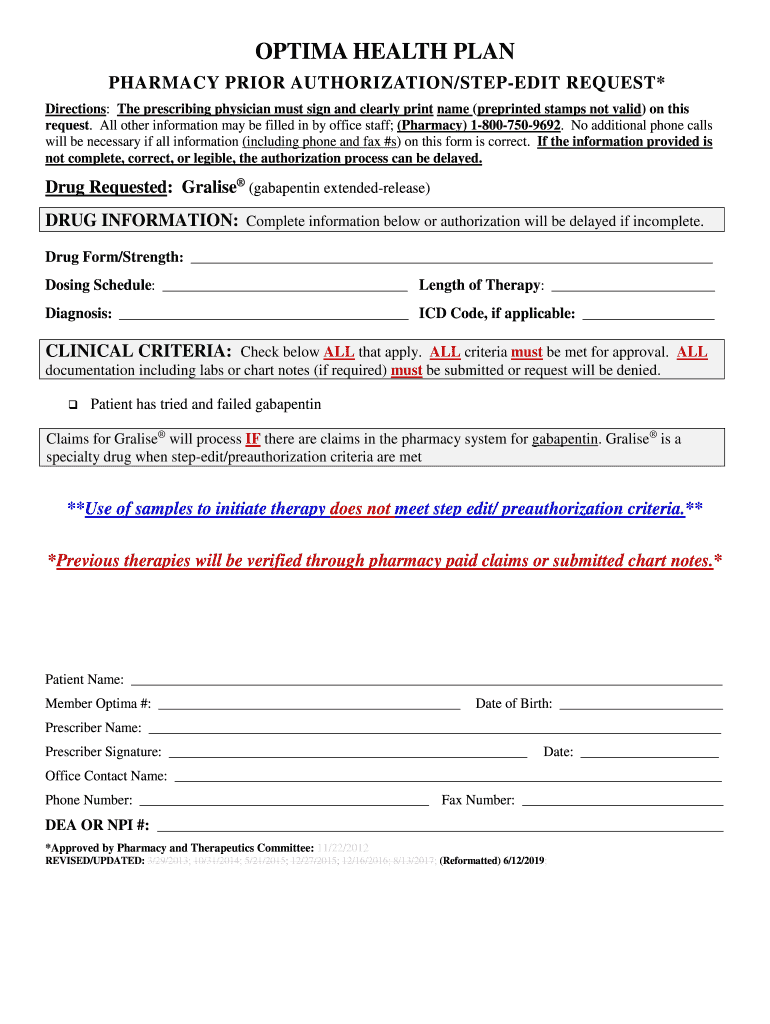
Fillable Online Optima Medicaid Prior Authorization Form Outline of
Select type of account and. Others are added as they become. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Member must be eligible at the time services are rendered. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to:
20212024 OH CareSource Medicaid Provider Prior Authorization Request
Services must be a covered health plan benefit and medically necessary with prior. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Some of the forms used by arkansas medicaid and its providers are available in electronic format. Member must be eligible at the time services are rendered. Others are added.
Free Arkansas Medicaid Prior (Rx) Authorization Form PDF eForms
Others are added as they become. Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. Select type of account and. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal.
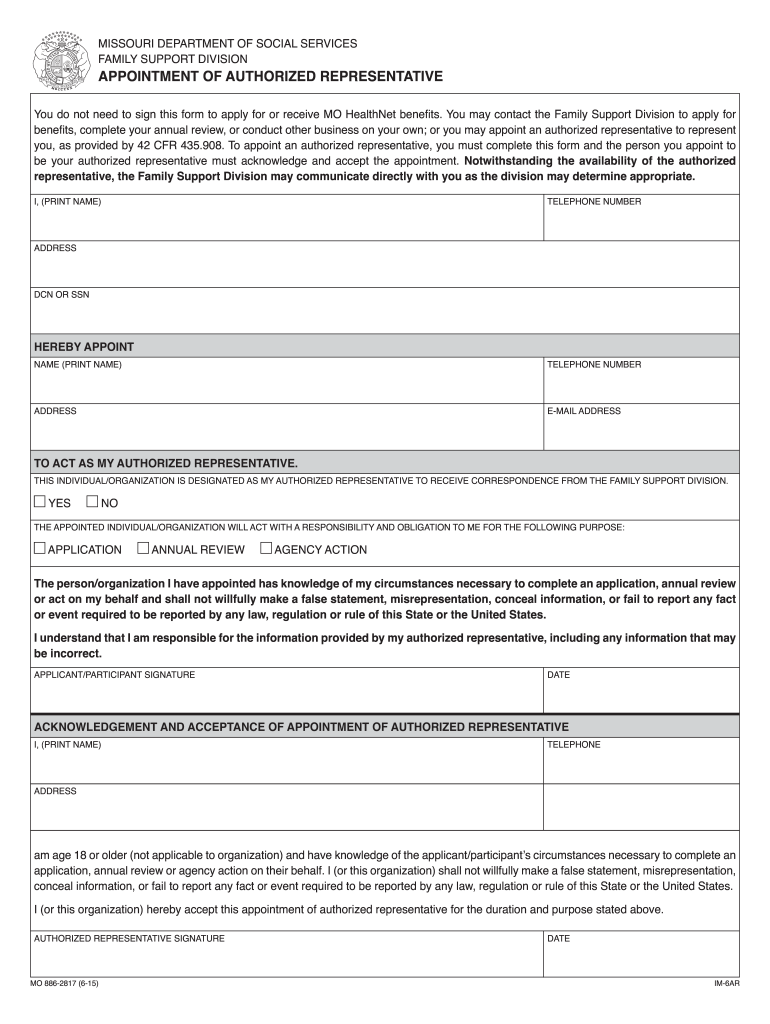
Medicaid authorized representative form Fill out & sign online DocHub
Select type of account and. Member must be eligible at the time services are rendered. Some of the forms used by arkansas medicaid and its providers are available in electronic format. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Others are added as they become.
DMS2692 Arkansas Medicaid
Select type of account and. Others are added as they become. Services must be a covered health plan benefit and medically necessary with prior. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Some of the forms used by arkansas medicaid and its providers are available in electronic format.
Medication Prior Authorization Request Form UnitedHealthcare Fill Out
Services must be a covered health plan benefit and medically necessary with prior. Member must be eligible at the time services are rendered. Select type of account and. Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal. Some of the forms used by arkansas medicaid and its providers are available in.
20202024 Form AR Medicaid Prior Authorization Request Fill Online
Others are added as they become. Services must be a covered health plan benefit and medically necessary with prior. Some of the forms used by arkansas medicaid and its providers are available in electronic format. Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Member must be eligible at the time services are rendered.
Some Of The Forms Used By Arkansas Medicaid And Its Providers Are Available In Electronic Format.
Arkansas medicaid prescription drug program statement of medical necessity prior authorization request fax form to: Services must be a covered health plan benefit and medically necessary with prior. Select type of account and. Member must be eligible at the time services are rendered.
Others Are Added As They Become.
Learn how to create, view, and request reconsideration or extension for prior authorization requests on the provider portal.